"I have true faith in my colleagues and I take heart from their calm determination and quiet courage. The usual petty grumbles and disagreements have been put aside, hopefully for good. We will need each other in these times to come and I know that we will work together to the best of our ability"
An Anonymous UK respiratory consultant who works across a number of hospitals.
COVID 19 ADVICE AND GUIDANCE FOR DOCTORS
The novel coronavirus (nCoV), named COVID-19, is part of a larger family of contagions. COVID 19 typically spreads from one person to another via respiratory droplets that are produced during coughing and sneezing, either directly in the air, or on surfaces.
Due to their close and prolonged contact with patients, doctors and healthcare workers may also be susceptible to aerosol transmission, and there is growing evidence of fecal-oral transmission, this is when the virus is shed in feces then ingested as a result of inadequate hand-washing or contaminated food and water.
COVID-19 was officially declared by The World Health Organization (WHO) as a pandemic on 12 March 2020. By this time doctors across the world were caring for patients at considerable risk to themselves. This article seeks to offer essential guidance and advice for doctors, many who face the most challenging personal and professional period of their careers.
WHO provide clear and detailed information, both on their website and as PDFs:
COVID-19 WHO Technical Guidance
Download the WHO Technical Guidance
The illustration below is an overview of the symptoms associated with COVID 19.
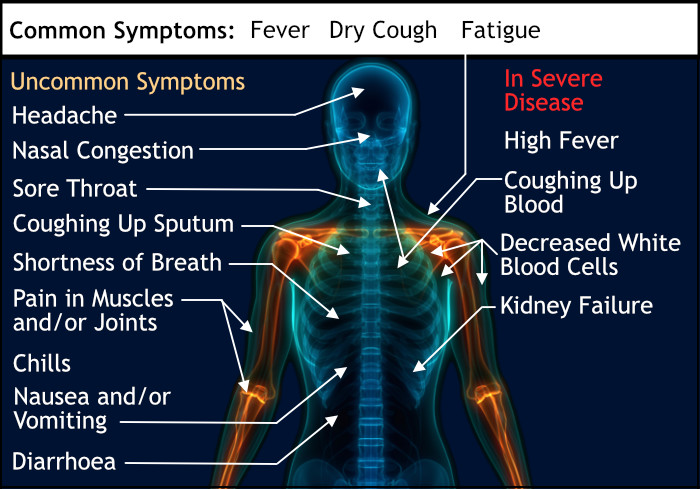
Image text with thanks to Mikael Häggström, M.D.
· Wash hands frequently with water and soap or hand-sanitizing gel.
· Maintain social distancing. Keep a distance of 1 metre (3 feet) between yourself and anyone who is coughing or sneezing.
· Avoid touching eyes, nose, and mouth.
· Follow respiratory hygiene: cover your mouth and nose with your bent elbow or tissue when you cough or sneeze, then dispose of the used tissue immediately.
· Seek medical care early if you have a fever, cough, or difficulty breathing
· Stay informed and follow advice given by your health-care provider, national and local public health authority.
COVID-19 impacts the elderly and those with pre-existing health conditions most severely.
Ensure your place of work is following the WHO guidelines:
It is crucial that doctors and medical staff are given the appropriate level of protection as they treat patients who may transmit COVID-19.
The first and most important step is to ensure that regular tests for the virus are made available, and whenever doctors request them. This not only ensures patients are better protected and the transmission of the virus is generally reduced, but regular testing also serves to strengthen the confidence of doctors who may otherwise be overexposed which may lead to a more significant and serious immune response.
Frequent testing for COVID-19 is recommended by WHO as it is not only a highly effective mechanism that places a break on the general transmission of the virus, it ensures doctors continue their work, certain in the knowledge they are not infecting others.
Personal protective equipment (PPE) is a crucial element in the reduction of transmission of the virus.
Doctors directly treating COVID-19 patients must be equipped with the appropriate level of protection. An N95 respirator if available, or at the very least an FFP3 medical mask, disposable full body gown tied at the back, gloves pulled over the gown sleeves, and preferably a full face plastic face shield (or goggles at a minimum).
Loosely fitting surgical masks will offer protection from large droplets. In comparison, a tight fitting FFP3 medical mask can filter up to 95% of small particles. Respirators are designed to be reused, however surgical and FFP3 medical masks are disposable. If masks are re-used because of short supply (it may appear a used mask is better than no mask), they must be set aside without use for at least 72 hours as the virus will not maintain its presence after this period. Re-use is not good practice however as other contaminates may be present in the mask as a result of use. Disposable equipment is intended for only a single use.
Some patients may require advice about how best to handle food to reduce the risk of catching or passing on Covid 19. Two authorities on food safety relating to Covid 19 follow.
The European Food Safety Authority on Covid 19
The FAO at the UN (Food and Agriculture Organization of the United Nations) also provides valuable information that can be downloaded as a PDF:
There are several strategies doctors can adopt that will reduce virus transmission.
Effective isolation procedures are not only important for treating patients with COVID-19 so that the transmission of the virus is reduced, doctors face potential infection from patients being treated for unrelated illness and injury as they may also carry the virus. To reduce the spread of the virus, phone calls and eConsultations should therefore be routinely offered in strong preference to face to face appointments.
Doctors have families. They may have partners, children, siblings, parents, and extended family members, some of whom may require special consideration or care like older members. Doctors are often required to work anti-social and long hours, and this places additional strain on family life and commitments. As COVID-19 results in significant additional demands on doctors, the following issues should be frequently discussed both in a family setting and at the doctor's place of work.
Social and Emotional Support: it is especially important in times of intense pressure and stress that doctors are encouraged to frequently share their concerns and experiences. Acts of sharing reduce the likelihood of burnout and a feeling of being overwhelmed. Sharing with family and colleagues is a crucial coping tool. Special care should be focused on those doctors who appear to be more socially isolated.
Balancing Family Responsibilities and Work: doctors may have children, parents, or other family members they have responsibilities for. It is important doctors feel they can meet both the needs of their family, and their work. During demanding and challenging periods, practice and hospital management should be especially focused on ensuring doctors are not given too much so as to decrease the quality and efficacy of their work. It is critical that doctors do not experience a tipping point when they feel overwhelmed and unable to function effectively. Apart from the negative impact this has on doctors, this also fails the patient's interests and undermines healthcare provision at a time of great demand.